Items filtered by date: February 2024
Unraveling the Mystery of Bunions

Hallux valgus, commonly known as a bunion, is a medical condition that affects the joint at the base of the big toe. This condition occurs when the big toe deviates towards the smaller toes, causing a bony protrusion on the side of the foot. Bunions can result from various factors such as genetics, improper footwear, and structural foot abnormalities. Symptoms of hallux valgus include pain, swelling, and redness around the big toe joint, often aggravated by wearing tight or ill-fitting shoes. As the bunion progresses, it may lead to difficulty in finding comfortable footwear, corns or calluses, and restricted joint movement. While conservative measures like wearing proper footwear and orthotic inserts may provide relief, severe cases may require surgical intervention to correct the deformity and alleviate symptoms. Understanding hallux valgus and its symptoms is critical for early intervention and effective management, promoting foot health and overall well-being. If you have developed a bunion, it is strongly suggested that you consult a podiatrist who can offer you effective relief methods.
If you are suffering from bunion pain, contact Edward S. Pozarny DPM of Arlington Podiatry Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in Arlington, VA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
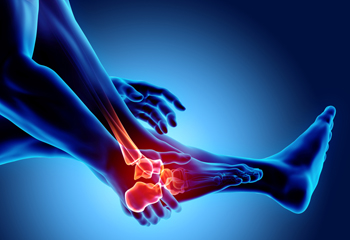
Pain and Foot Fractures

Treatment for a broken foot typically involves rest, elevation, and taking anti-inflammatory medications to manage pain and swelling. Healing times differ depending on the severity of the break. Symptoms also vary, including pain, difficulty moving the foot, and tenderness. Differentiating between a broken foot and a sprain can be challenging, but fractures generally result in more intense and continuous pain. Treatment options include immobilization with a cast, surgical intervention for severe cases, and rehabilitation exercises. Prevention measures include wearing appropriate footwear and maintaining bone health with a balanced diet and regular exercise. If you have sustained a foot fracture, it is suggested that you schedule an appointment with a podiatrist as quickly as possible. Prompt medical attention and adherence to treatment guidelines are essential for successful healing.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact Edward S. Pozarny DPM from Arlington Podiatry Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our office located in Arlington, VA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Definition and Symptoms of a Diabetic Foot Wound
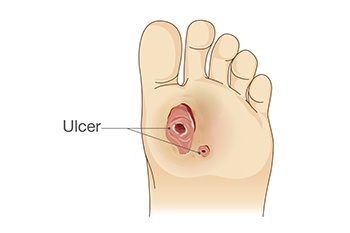
A diabetic foot wound refers to an open sore or ulcer that develops on the foot of individuals with diabetes, typically due to a combination of factors including neuropathy, poor circulation, and impaired wound healing. Neuropathy, a common complication of diabetes, causes nerve damage that diminishes sensation in the feet, making individuals less aware of injuries or pressure points that can lead to wounds. Poor circulation, another consequence of diabetes, reduces blood flow to the feet, hindering the delivery of oxygen and nutrients necessary for wound healing. These factors, coupled with compromised immune function, increase the risk of infections and slow the healing process. Symptoms of diabetic foot wounds may include redness, swelling, warmth, drainage, and foul odor. Recognizing these signs is crucial for prompt intervention and prevention of complications such as infections and amputations. If you have diabetes and have developed a foot wound, it is strongly suggested that you are under the care of a podiatrist who can provide you with the proper wound care.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Edward S. Pozarny DPM from Arlington Podiatry Center. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Arlington, VA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Types and Alleviation Strategies for Foot Arthritis
Foot arthritis, a multifaceted condition, manifests in various ways, each presenting distinct challenges for those grappling with joint inflammation in the feet. Osteoarthritis, the most common form, results from wear and tear on the joints, causing pain and stiffness. Rheumatoid arthritis, an autoimmune disorder, targets the joints and may lead to deformities in the feet. Gout, characterized by the accumulation of uric acid crystals, induces sudden and severe pain. Recognizing the specific type of foot arthritis is essential for implementing targeted relief methods. While medications are common approaches to treatment, lifestyle modifications such as maintaining a healthy weight and choosing supportive footwear can help to alleviate symptoms. Resting the feet and engaging in gentle exercises can provide relief. Foot arthritis can cause discomfort, and if you are suffering from this condition, it is suggested that you visit a podiatrist who can guide you toward effective relief methods.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact Edward S. Pozarny DPM from Arlington Podiatry Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a term that is commonly used to describe joint pain. The condition itself can occur to anyone of any age, race, or gender, and there are over 100 types of it. Nevertheless, arthritis is more commonly found in women compared to men, and it is also more prevalent in those who are overweight. The causes of arthritis vary depending on which type of arthritis you have. Osteoarthritis for example, is often caused by injury, while rheumatoid arthritis is caused by a misdirected immune system.
Symptoms
- Swelling
- Pain
- Stiffness
- Decreased Range of Motion
Arthritic symptoms range in severity, and they may come and go. Some symptoms stay the same for several years but could potentially get worse with time. Severe cases of arthritis can prevent its sufferers from performing daily activities and make walking difficult.
Risk Factors
- Occupation – Occupations requiring repetitive knee movements have been linked to osteoarthritis
- Obesity – Excess weight can contribute to osteoarthritis development
- Infection – Microbial agents can infect the joints and trigger arthritis
- Joint Injuries – Damage to joints may lead to osteoarthritis
- Age – Risk increases with age
- Gender –Most types are more common in women
- Genetics – Arthritis can be hereditary
If you suspect your arthritis is affecting your feet, it is crucial that you see a podiatrist immediately. Your doctor will be able to address your specific case and help you decide which treatment method is best for you.
If you have any questions, please feel free to contact our office located in Arlington, VA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
